Educational Outcomes: Outcomes Breaking New Reports
 OC/Twitter Blast on MS: week of January 6, 2014. JBLeffler.
OC/Twitter Blast on MS: week of January 6, 2014. JBLeffler.
At 4 Months Follow Up, 100% of Chair Summit Participants Who See Patients with MS Remain Committed to Increasing and Improving Their Use of Evidence-Based Tools to Monitor Disease Symptoms
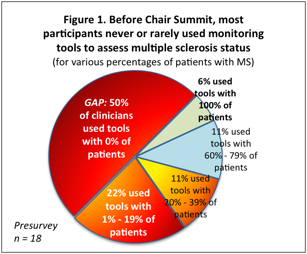
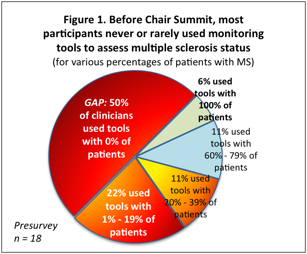
In a pre-activity survey of participants in the 5th Annual Chair Summit in 2012, nearly three quarters of participants reported that they rarely (22%) or never (50%) used evidence-based assessment tools to monitor disease progression in their patients with multiple sclerosis (MS). A large gap in the use of evidence-based assessment tools was illustrated by the 94% of attendees who were NOT using validated office tools to assess disease activity, mobility issues, and the disease course in 100% of their patients with MS (see Figure 1); this despite international guidelines for the use of validated tools.1 Educational planners chose this performance measure for follow-up assessments. Long-term outcomes surveying provided 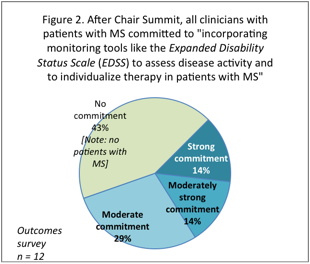 context for 2012 content planning and showed a performance improvement in MS care: all respondents “recommended exercise and nonpharmacological approaches—in addition to pharmacotherapy—to patients with multiple sclerosis who have cognitive impairment” in 60% – 100% of their patients with MS. Because cognitive impairment and other quality of life concerns affect patient outcomes,2 measuring the use of tools to assess MS symptoms was seen as an appropriate step in explaining the remaining gaps seen in earlier treatment-related educational outcomes. In fact, practice guidelines from the American Academy of Neurology (AAN), the European Federation of Neurological Societies (EFNS), and the United Kingdom National Institute for Health and Clinical Excellence (NICE) include the use of physician- and patient-reported outcome tools,1 providing CME participants with a quality measure to attain in MS care. Further making the educational content on guidelines in MS appropriate for Chair Summit participants, 72% of targeted clinicians indicated this large, pre-activity performance gap in using disease assessment and monitoring tools. Retention of content on monitoring tools for MS was seen at four months, in which clinicians correctly identified the “ABC” tool for clinical monitoring in MS as an assessment tool for “allodynia, bladder problems, and cognitive impairment.”
context for 2012 content planning and showed a performance improvement in MS care: all respondents “recommended exercise and nonpharmacological approaches—in addition to pharmacotherapy—to patients with multiple sclerosis who have cognitive impairment” in 60% – 100% of their patients with MS. Because cognitive impairment and other quality of life concerns affect patient outcomes,2 measuring the use of tools to assess MS symptoms was seen as an appropriate step in explaining the remaining gaps seen in earlier treatment-related educational outcomes. In fact, practice guidelines from the American Academy of Neurology (AAN), the European Federation of Neurological Societies (EFNS), and the United Kingdom National Institute for Health and Clinical Excellence (NICE) include the use of physician- and patient-reported outcome tools,1 providing CME participants with a quality measure to attain in MS care. Further making the educational content on guidelines in MS appropriate for Chair Summit participants, 72% of targeted clinicians indicated this large, pre-activity performance gap in using disease assessment and monitoring tools. Retention of content on monitoring tools for MS was seen at four months, in which clinicians correctly identified the “ABC” tool for clinical monitoring in MS as an assessment tool for “allodynia, bladder problems, and cognitive impairment.”
In follow-up assessments four months after the live activity, CMEO demonstrated that education on the use of tools that assess disease status did change clinicians’ attitudes: Every respondent who had patients with MS (57% of respondents) made moderate-to-strong commitments to using tools like the Expanded Disability Status Scale (EDSS). All other respondents stated that they did not currently have patients with MS, and accordingly did not commit to this performance measure (n = 12; see Figure 2). Therefore, these findings showed that 100% of Chair Summit participants who see patients with MS could be expected to improve their use of evidence-based tools to monitor disease symptoms. Follow-through on this commitment should help clinicians individualize patients’ treatment needs and therefore promote patients’ adherence to disease-modifying therapy.
References
- Trisolini MG. Comparison of multiple sclerosis guidelines underscores need for collaboration [expert commentary]. Agency for Healthcare Research and Quality (AHRQ) Website. http://www.guideline.gov/expert/expert-commentary.aspx?id=16443. Published December 8, 2008. Accessed July 2, 2013.
- Lobentanz IS, Asenbaum S, Vass K, et al. Factors influencing quality of life in multiple sclerosis patients: disability, depressive mood, fatigue and sleep quality. Acta Neurol Scand. 2004;110:6-13. PMID: 15180801.
How to Cite This Document
CME Outfitters, LLC. CME Activity Outcomes Report and Interpretation: Multiple Sclerosis Sessions at the 4th Annual Chair Summit [data on file]. Bethesda, MD: CME Outfitters; 2013.
This document was last modified on:


 OC/Twitter Blast on MS: week of January 6, 2014. JBLeffler.
OC/Twitter Blast on MS: week of January 6, 2014. JBLeffler.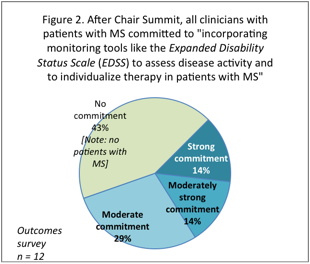 context for 2012 content planning and showed a performance improvement in MS care: all respondents “recommended exercise and nonpharmacological approaches—in addition to pharmacotherapy—to patients with multiple sclerosis who have cognitive impairment” in 60% – 100% of their patients with MS. Because cognitive impairment and other quality of life concerns affect patient outcomes,2 measuring the use of tools to assess MS symptoms was seen as an appropriate step in explaining the remaining gaps seen in earlier treatment-related educational outcomes. In fact, practice guidelines from the American Academy of Neurology (AAN), the European Federation of Neurological Societies (EFNS), and the United Kingdom National Institute for Health and Clinical Excellence (NICE) include the use of physician- and patient-reported outcome tools,1 providing CME participants with a quality measure to attain in MS care. Further making the educational content on guidelines in MS appropriate for Chair Summit participants, 72% of targeted clinicians indicated this large, pre-activity performance gap in using disease assessment and monitoring tools. Retention of content on monitoring tools for MS was seen at four months, in which clinicians correctly identified the “ABC” tool for clinical monitoring in MS as an assessment tool for “allodynia, bladder problems, and cognitive impairment.”
context for 2012 content planning and showed a performance improvement in MS care: all respondents “recommended exercise and nonpharmacological approaches—in addition to pharmacotherapy—to patients with multiple sclerosis who have cognitive impairment” in 60% – 100% of their patients with MS. Because cognitive impairment and other quality of life concerns affect patient outcomes,2 measuring the use of tools to assess MS symptoms was seen as an appropriate step in explaining the remaining gaps seen in earlier treatment-related educational outcomes. In fact, practice guidelines from the American Academy of Neurology (AAN), the European Federation of Neurological Societies (EFNS), and the United Kingdom National Institute for Health and Clinical Excellence (NICE) include the use of physician- and patient-reported outcome tools,1 providing CME participants with a quality measure to attain in MS care. Further making the educational content on guidelines in MS appropriate for Chair Summit participants, 72% of targeted clinicians indicated this large, pre-activity performance gap in using disease assessment and monitoring tools. Retention of content on monitoring tools for MS was seen at four months, in which clinicians correctly identified the “ABC” tool for clinical monitoring in MS as an assessment tool for “allodynia, bladder problems, and cognitive impairment.”



